The case for more geriatricians: Strengthening the workforce to care for an ageing population
This report is intended to start the conversation about the workforce needed to provide high-quality care for the ageing population with increasingly complex needs. It explains why training, recruiting and retaining geriatricians should be a priority, estimates how many geriatricians are needed to provide safe and effective care for older people, and outlines some of the structural barriers that currently prevent recruitment. It concludes with six calls from the BGS for Governments across the UK.
Introduction
The NHS workforce is in crisis – there are currently not enough people with the right skills to provide the high-quality care that the population needs and expects.
Healthcare professionals currently working within the NHS are exhausted and burnt out as a result of working in conditions that are not conducive to providing excellent care. At the time of writing, unresolved industrial action is affecting several disciplines. The NHS is losing considerable numbers of staff with many leaving healthcare entirely or choosing to take up higher-paid positions in other countries. The end result is that patients are waiting longer for treatment only to receive a level of care that is inferior to what they would expect and to what their clinicians would wish to provide. As older people are the biggest user group of health and social care, they are the group who are most frequently affected by delays in access to care and suboptimal experience of care.
This crisis will not be fixed by short term measures that address just one part of the problem. To provide high-quality healthcare for all people in the UK, when and where they need it, requires strategic, system-wide workforce planning and investment in creative and sustainable workforce solutions. This includes improving terms and conditions for NHS and social care staff in order to make health and social care attractive career options and to be able to recruit and retain more staff at all levels. Action on terms and conditions should be complemented by workforce education and development so that more of our current and future workforce have the right skills to care for the biggest group using health and care services: older people. However, central to the solution must be recruiting more people. The British Geriatrics Society (BGS) stands with many other organisations in making the case for more health and care staff. We believe that concerted action to recruit and train more people with the skills required for a rapidly ageing population is central to having a sustainable workforce that is fit for the future. In this paper, we take that argument one step further in putting a number on how many more geriatricians are needed to work in the NHS to meet the needs of an ageing population with increasingly complex needs.
We believe that concerted action to recruit and train more people with the skills required for a rapidly ageing population is central to having a sustainable workforce that is fit for the future.
Care for older people is largely delivered by multidisciplinary teams, whether in acute, community or primary care. However, these teams need the leadership of geriatricians, who are expert in balancing the harms and benefits of interventions for older people with complex needs as a result of frailty and multiple conditions. Therefore, recruitment of geriatricians is only one part of a wider capacity challenge, but it is a vital one to address as part of a strategic approach to workforce planning.
This paper is intended to start the conversation about the workforce needed to provide high-quality care for the ageing population with increasingly complex needs. The paper explains why training, recruiting and retaining geriatricians should be a priority, estimates how many geriatricians are needed to provide safe and effective care for older people, and outlines some of the structural barriers that currently prevent recruitment. The document concludes with six calls for Governments across the UK. There are limitations to this paper, which we acknowledge. However, it is clear that national and local strategic workforce plans must address the need for more geriatricians alongside investment in multidisciplinary teams and in upskilling the entire workforce to care for older people with frailty.
Context for prioritising older people’s care
Older people, particularly those with frailty, use health and care services more than any other group.
The winter of 2022/23 saw severe and sustained pressures on the health and social care system, with unprecedented delays for ambulances, extremely long waits on trolleys in emergency departments and delayed transfers of care once people were ready for discharge. At one point during the winter, around 13,000 people in England who had been designated ready for discharge from hospital were waiting in hospital either for a social care package or for rehabilitation.1,2 This is around 10% of the acute hospital bed base. Most of those delayed were older people living with frailty.
Frailty affects up to half of the population over 85 years and is estimated to cost UK healthcare systems £5.8 billion per year before the costs of social care are taken into account.3 The number of people aged over 85 in the UK is set to double by 2045.4 When one considers that it takes on average 16 years from entry to medical school to train a consultant geriatrician5 it is apparent that we need action now to ensure that we have enough doctors with specialist skills in the complex needs of older people.
It is clear from last winter that the health and social care system needs to work better for older people with frailty, if it is to function at all. Some of the solutions to the crisis of last winter lie outside of the NHS. A significant amount of harm could have been avoided if social care services were adequately staffed and funded and if procedures for identifying and using social care capacity were harmonised and streamlined across the country.
Effective care for older people with frailty applies the evidence-based principles of Comprehensive Geriatric Assessment (CGA). This approach involves multidisciplinary assessment of physical, cognitive, functional, psychological, and social issues to identify personalised priorities which form the basis of an iterative care and support plan, with interventions delivered by a team of health and social care professionals.6,7
The policy levers to enable this approach for older people in the community were outlined in the Ageing Well programme of the NHS England Long Term Plan.8 Two of the initiatives within the Ageing Well programme – Enhanced Health in Care Homes and Urgent Community Response – are being implemented. A third – Anticipatory Care – has been renamed as Proactive Care, but formal launch is awaited pending funding announcements. An additional initiative, announced during winter 2022/23 and underway using the principles of CGA, is the Frailty Virtual Ward (Hospital at Home) service.9 Rehabilitation has largely not been considered as part of the Ageing Well programme. Although some urgent community response and Hospital at Home services may include an element of short term rehabilitation, there has been a lack of investment in the rehabilitation capacity required to restore functional ability and reduce future demand for health and care.
In acute hospitals, the evidence base for services which use CGA is increasingly robust.10 There is substantial focus on establishing acute frailty services and same day emergency care (SDEC), surgical liaison services for older people, oncogeriatric services, and in further expanding orthogeriatric models of care to ensure that all older people experiencing acute trauma receive optimised inpatient medical care, enabling the best chance of recovery.
Effective care for older people with frailty applies the evidence-based principles of Comprehensive Geriatric Assessment (CGA). This approach involves multidisciplinary assessment of physical, cognitive, functional, psychological, and social issues to identify personalised priorities which form the basis of an iterative care and support plan, with interventions delivered by a team of health and social care professionals.6,7
Limitations of this paper
While this paper makes a strong case for increasing consultant geriatrician numbers, it is important to note that this alone will not be sufficient to ensure that older people’s healthcare is fully resourced in the future.
Older people’s healthcare is multidisciplinary. Increasing geriatrician numbers will help, but without a similar increase in specialist nurses, allied health professionals, physician associates, specialist pharmacists and others, the workforce will remain under-resourced.
This paper focuses on doctors because there is workforce data available for doctors. The Royal College of Physicians’ (RCP) census provides data on the number of consultants currently in post in each specialty and expected retirements. This allows us to make estimates of the numbers of doctors who will be in post in the coming years and therefore how many new doctors will be needed. Similar data does not exist for the other professions. The BGS is eager to work with relevant Royal Colleges and other specialist societies to explore how this data can be obtained. In the meantime, we have focused this paper on the medical workforce and acknowledge that this illustrates a partial solution.
As stated, the figures that this paper uses are based on the RCP census of consultants. These figures do not include geriatric medicine trainees or SAS grade doctors, who play a crucial role in care for older people.
This paper suggests numbers for the whole of the UK and is not broken down into the needs of each of the four nations. While the RCP census can be broken down by nation and specialty, we are conscious of the small number of respondents from some nations. For example, only 13 geriatricians responded to the survey from Northern Ireland. As such, we are cautious about making recommendations on a per nation basis and have kept our numbers broad.
Older people’s healthcare is multidisciplinary. Increasing geriatrician numbers will help, but without a similar increase in specialist nurses, allied health professionals, physician associates, specialist pharmacists and others, the workforce will remain under-resourced.
The numbers
According to the 2021 Royal College of Physicians Census, there are currently 1,900† fully trained consultant geriatricians in the UK.11
These figures do not include non-consultant doctors including Higher Specialty Trainees and SAS doctors, who play a vital role in the delivery of older people’s healthcare across various settings. They also do not include doctors from other specialties for whom older people form a significant proportion of their patient group (e.g. GPs and stroke physicians).
While the rate of consultant geriatricians is not uniform across the UK, we have highlighted the number of geriatricians in three separate parts of the UK, as illustrated in Table 1. We have chosen to highlight the areas where the number of geriatricians per head of older population is both highest (London) and lowest (East Midlands) and Scotland, to provide a comparator between these two extremes.
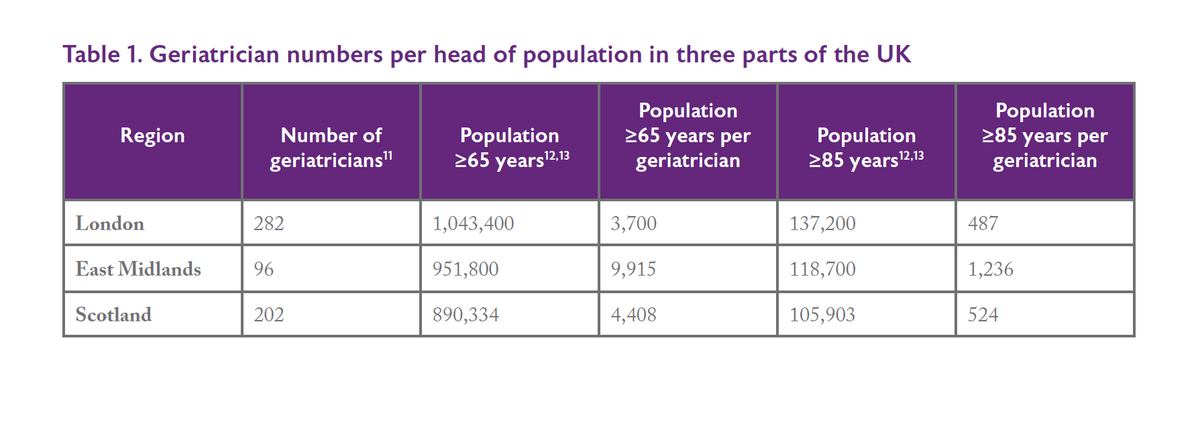 We appreciate that these do not provide perfect comparisons as these areas have different populations and they do not take into consideration the complexities of covering rural and remote locations. However, the figures do provide a starting point and reflect our discussions with the BGS membership. In London we have seen rapid expansion of specialist front-door frailty, surgical liaison, orthogeriatric and community services. Scotland has been a pioneer in the Hospital at Home movement and other models of care in the community. Colleagues in the East Midlands, meanwhile, report feeling overwhelmed and unable to keep pace with the demand for service expansion in both acute and community settings.
We appreciate that these do not provide perfect comparisons as these areas have different populations and they do not take into consideration the complexities of covering rural and remote locations. However, the figures do provide a starting point and reflect our discussions with the BGS membership. In London we have seen rapid expansion of specialist front-door frailty, surgical liaison, orthogeriatric and community services. Scotland has been a pioneer in the Hospital at Home movement and other models of care in the community. Colleagues in the East Midlands, meanwhile, report feeling overwhelmed and unable to keep pace with the demand for service expansion in both acute and community settings.
Current NHS policy objectives, across the four nations, include Virtual Wards (Hospital at Home), an increased focus on rehabilitation and intermediate care, implementation of front door frailty services, and pre- and peri-operative support for older people with frailty. To achieve this wide scope of areas of service delivery around the country, staffing levels must come up to those seen in the most highly capitated areas for geriatricians. These are the only parts of the UK where all these competing demands have been met, successfully, in parallel.
If we want to emulate the progress in scaling up evidence-based models of care seen in the most highly-capitated parts of the country, then we need to raise the number of specialist geriatricians employed elsewhere to this level – referred to hereafter as “the national benchmark”. We would suggest that a ratio of one geriatrician to every 500 people aged over 85 is a benchmark to strive for. This will enable the NHS to develop and deliver evidence-based models of care for older people across the whole system.
It is possible to estimate how many consultant geriatricians would be required to achieve this national benchmark in order to enable a similar level of specialist-led services for older people across the UK (Table 2).
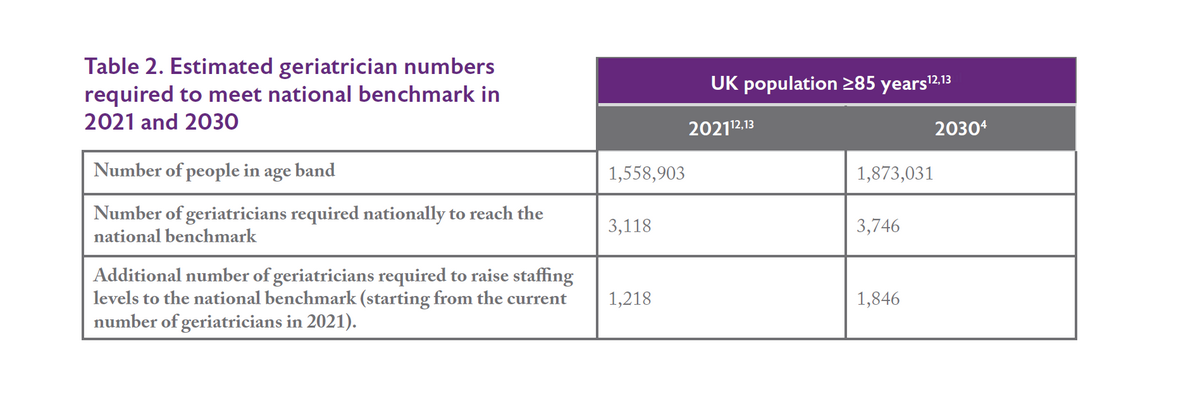
Thus, an additional 1,218 geriatricians would be currently required, nationally, to ‘level up’ to the national benchmark in order to meet the current demand for specialist services for older people. Projected numbers required by 2030 are 1,846.
This is a conservative estimate that does not take into consideration specific local challenges of rurality and deprivation. These workforce requirements may be altered by development of nurse and AHP consultants and advanced practitioner posts – but such posts are already well developed in the parts of the country more highly capitated for consultant geriatricians. We do not believe, therefore, that these developments will change our estimates by a significant margin. It is important that these advanced nursing and therapy roles continue to be developed and recruited to, alongside additional medical recruitment. It is also important to note that these estimates are based on consultant geriatricians only – recruitment into other medical roles such as SAS doctors will be necessary as well to ensure that older people are able to access the care that they need. It is also necessary to increase the skills and knowledge of the workforce in other specialties to ensure that healthcare professionals across the NHS have the skills they need to care for older people with frailty. With the exception of those working in paediatric and maternity services, most healthcare professionals will care for older people more than any other age group.
These estimates require further inflation to take account of expected retirements. The RCP census suggests that 821 geriatricians will reach retirement age in the next decade. Accounting for the need to replace the retiring workforce, while addressing the regional inequities in consultant geriatric medical provision outlined above, would require training an additional 2,667 geriatricians by 2030. This is an indicative figure and does not allow for the anticipated increase in flexible and Less than Full Time (LTFT) working, which currently 25% of the geriatric medicine consultant workforce undertake. A BGS survey in summer 2022 suggested that 37% of geriatric medicine trainees work flexibly. Only 15% of higher specialty trainees across all specialties work flexibly, suggesting that this is more common in geriatric medicine.5 This is to be welcomed and encouraged as allowing flexible working boosts retention and improves mental health. However, it must be considered when planning for future workforce requirements. Between 2011 and 2018, more than 56,000 people stopped working for the NHS in England, citing lack of work life balance as the reason.14
Currently 43% of consultant geriatricians contribute to the acute unselected medical take.5 This will involve seeing both older patients with frailty, and younger people who they review in their capacity as general physicians. This is considerably higher than other specialties, with 30% of consultants overall and only 10% of consultant cardiologists contributing to the unselected medical take. We would envisage a need for geriatricians to continue to contribute to the acute take.5 Our current calculations are based upon the assumption that this will be at the current level of commitment. Clearly, if other medical specialties take on more acute general (internal) medicine work, then this will have implications for the figures presented here. It is important that additional geriatrician posts developed as part of workforce changes are not consumed entirely by commitments to general (internal) medicine. These posts must have protected time dedicated to the delivery of frailty care through the multiple novel approaches advocated in national policy documents and initiatives.
These calculations come with so many caveats because they are based on voluntary returns to an annual census conducted by the Royal College of Physicians. Clearly, the NHS needs to establish better workforce data for sustainable approaches to workforce planning in the future. We cannot, however, afford to wait for such data if we are to deliver the care that our older patients need. This is why the BGS has chosen to act now.
† It is important to note that these numbers refer to the headcount from the RCP census and not whole-time equivalent roles.
Barriers
Currently not enough geriatricians are being trained to meet these figures.
National Training Number (NTN) data indicates 118 new geriatricians are trained each year. According to a BGS survey conducted in summer 2022, 37% of geriatric medicine trainees work LTFT. This would suggest that around 43 of the 118 new geriatricians each year work LTFT – we estimate, therefore that 105 full-time equivalents are currently in NTNs, based upon a conservative assumption that most LTFTs work circa 0.7 FTE. Of those who work LTFT, across both consultant and trainee posts, the majority are women. Geriatric medicine has a slightly higher proportion of women than is typical across medicine and this is likely to continue as there are currently more female than male trainees.5 This shows the massive disparity between current training provision in geriatric medicine and the scale of the need.
The specialty is increasingly popular for medical trainees. In 2017, 213 applicants applied for 152 geriatric medicine ST4 posts and in 2022, 343 applicants applied for 155 posts. This equates to 2.2 applicants for every ST4 post in 2022 compared to 1.4 applicants for each post in 2017.15 Similarly, in 2022 there were 4,008 applicants for 1,639 IMT posts, an increase from 2,343 applicants for 1,657 posts in 2017.16 This equates to 2.45 applicants for every post in 2022 and 1.41 applications per post in 2017. While there has been an increase in the number of medical school places in recent years, this is yet to be reflected in an increase in foundation/IMT/ST posts, creating the bottleneck described above. It would be feasible to double the number of registrar posts in geriatric medicine immediately and expect to recruit into them.
Clearly, sustainable training at such levels is dependent upon sufficient doctors coming through earlier stages of training. This means a further increase in medical school places to ensure that enough doctors are being trained within the UK to meet the needs of the NHS. Currently many applicants for posts are international medical graduates whose training needs may be different. Attracting international graduates can also have a detrimental impact on health systems in other countries who are not benefitting from the expertise of the doctors that their systems have trained. A further increase to medical school places would mean that the NHS could become less reliant on recruitment from other countries. The Royal College of Physicians has called for medical school places to be doubled from 7,500 to 15,00017 and the BGS supports and reiterates this call.
It is therefore necessary to tackle this issue as two separate strategies. There needs to be an increase in NTNs for geriatric medicine as well as an increase in posts at ST4 stage. In addition, a targeted recruitment drive would be required if we are to be more ambitious in our expansion of numbers.
The BGS calls on the Government to act on the following key areas
We need to make up the shortfall in consultant geriatricians, urgently.
To this end, the BGS calls for:
- A UK-wide target of one consultant geriatrician per every 500 people aged 85 and over to be used as the basis of consultant workforce and training projections.
- An urgent expansion of National Training Numbers in geriatric medicine to allow for the above. We estimate this will require an additional 300 geriatric medicine National Training Numbers per year to meet the proposed target by 2030, if recruitment were to start in 2024.
- An urgent increase in the number of ST4 geriatric medicine posts available to support the expansion in national training numbers.
- Detailed work to establish the number of additional training posts per annum on a deanery-by-deanery basis, with a view to meeting the proposed target across all deaneries by 2030.
- Continuous review of the above requirements taking account of the number of trainees in Less Than Full Time employment and the projections on numbers of geriatricians retiring.
- A national recruitment drive, highlighting the importance of geriatric medicine, and career opportunities within the specialty. This should complement materials focused on expanding the numbers of nurses, AHPs and ACPs choosing a career in older people’s healthcare.
Conclusion
It is clear to anyone working within health and social care that the status quo is not an option.
Older adults already comprise the majority of people who use health and care services and this is set to continue as the population ages and more people live longer with more complex needs.
The NHS was founded 75 years ago on the principle of free care at the point of delivery, funded by the taxpayer. Public support for this principle remains high18 but it is not deliverable without urgent action on the workforce. This paper makes the case for investment in training more geriatricians. This alone will not solve the crisis, but the crisis will not be solved without this investment.
References
References
Click to expand
- Schlepper L, Dodsworth E and Scobie S, 2023. Understanding delays in hospital discharge: Nuffield Trust QualityWatch Blog. Available at: www.nuffieldtrust.org.uk/news-item/understanding-delays-in-hospital-dis… (accessed 28 April 2023)
- Wise J. ‘Delayed discharge: One in six patients in hospital in England are medically fit to leave’. BMJ 2023;380:p578
- Han et al, 2019. ‘The impact of frailty on healthcare resource use: a longitudinal analysis using the Clinical Practice Research Datalink in England’, Age and Ageing. Sep 1;48(5):665-671
- Office for National Statistics, 2022. National Population Projections: 2020-based interim. Available at: www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/popu… (accessed 28 April 2023)
- British Geriatrics Society, 2022. The geriatric medicine workforce 2022. Available at: www.bgs.org.uk/GMworkforce22 (accessed 28 April 2023)
- British Geriatrics Society, undated. CGA in acute settings. Available at: www.bgs.org.uk/topics/cga-in-acute-settings (accessed 28 April 2023)
- British Geriatrics Society, undated. CGA in community settings. Available at: www.bgs.org.uk/topics/cga-in-community-settings (accessed 28 April 2023)
- NHS England, undated. NHS Long Term Plan: Ageing Well. Available at: www.longtermplan.nhs.uk/areas-of-work/ageing-well (accessed 28 April 2023)
- British Geriatrics Society, 2022. Bringing hospital care home: Virtual wards and Hospital at Home for older people with frailty. Available at: www.bgs.org.uk/virtualwards (accessed 28 April 2023)
- British Geriatrics Society, 2023. Joining the dots: A blueprint for preventing and managing frailty in older people. Available at: www.bgs.org.uk/Blueprint (accessed 28 April 2023)
- Royal College of Physicians, 2022. Working differently in the shadow of COVID-19: the UK 2021 census of consultant, high specialty trainees and SAS physicians. Available at: www.rcplondon.ac.uk/projects/outputs/working-differently-shadow-covid-1… (accessed 28 April 2023)
- Office for National Statistics, 2022. Population and household estimates, England and Wales: Census 2021. Available at: www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/popu… (accessed 28 April 2023)
- Scotland’s Census, 2011. Scottish Council Area 2011 by Age by Term-time Address. Available at: www.scotlandscensus.gov.uk/webapi/jsf/tableView/tableView.xhtml (accessed 28 April 2023)
- NHS England, 2020. We are the NHS: People Plan 2020/21 – action for us all. Available at: www.england.nhs.uk/wp-content/uploads/2020/07/We-Are-The-NHS-Action-For… (accessed 28 April 2023)
- NHS Physician Higher Specialty Training Recruitment, undated. Geriatric Medicine. Available at: https://phstrecruitment.org.uk/specialties/geriatric-medicine (accessed 28 April 2023)
- Health Education England, 2022. Competition ratios for 2022. Available at: https://medical.hee.nhs.uk/medical-training-recruitment/medical-special… (accessed 28 April 2023)
- Royal College of Physicians, 2022. RCP view on the NHS workforce: short- and medium-term solutions. Available at: www.rcplondon.ac.uk/guidelines-policy/rcp-view-nhs-workforce-short-and-… (accessed 28 April 2023)
- Buzelli L, Williamson S, Gardner T and Cameron G, 2023. Public perceptions of the NHS: a winter of discontent. Available at: www.health.org.uk/publications/long-reads/public-perceptions-of-the-nhs… (accessed 28 April 2023).
Contributors
Contributors
Click to expand
- Professor Adam Gordon, BGS President; Professor of Care of Older People, University of Nottingham; Consultant Geriatrician, University Hospitals of Derby and Burton NHS Foundation Trust
- Dr Amit Arora, BGS Vice President for Workforce; Regional Clinical Director, ECIST- NHS England
- Dr Katherine Chin, BGS Workforce Committee Junior Doctor Representative; Research and Teaching Fellow in Geriatric Medicine; Guy’s and St Thomas’ Hospital.
- Dr Tom Downes, Vice President Clinical Quality, BGS; Consultant Geriatrician and Clinical Lead for Quality Improvement, Sheffield Teaching Hospitals
- Sally Greenbrook, BGS Policy Manager
- Professor Anne Hendry, BGS Honorary Secretary; Honorary Professor, University of the West of Scotland
- Dr Amanda Koh, BGS Trainees’ Council Member; IMT2 trainee, Northwick Park Hospital
- Dr Sangam Malani, BGS Trainees’ Council Chair; ST5 Trainee in Geriatric Medicine.
- Sarah Mistry, BGS Chief Executive