Ahead of the Chancellor’s Autumn Statement on 17 November 2022, the BGS is calling for a renewed commitment to investing in health services for older people. The cost of living crisis is making life more difficult for people across the whole of society, as well as putting increased pressure on the NHS, a system already stretched to breaking point by the COVID pandemic.
In this challenging environment, we ask Governments across the UK to recognise and address the needs of the largest population group using health services. We urge them to maintain funding and continue the movement to bring care for older people closer to home as set out in the Long Term Plan in England, and equivalent strategies in Scotland, Wales and Northern Ireland.
Failure to invest in older people’s care is short-sighted and leads to poorer health at greater cost to the NHS. Investing in proactive care in the community and a sustainable social care solution frees up capacity in acute care to address the backlog of people waiting for the care they desperately need.
Ageing is an inevitable, universal process. Older people can be helped to live healthy lives and maintain independence longer with the right support and early intervention. Investing in such care and support improves health outcomes, saves money and relieves pressure on the health system. The BGS calls on Governments to commit to long term investment in older people’s care to ensure we can all live well into old age.
| We are highlighting key issues in older people’s care via a social media campaign. Over the next 8 days, we will promote via Twitter one statistic a day about older people’s health, and what the Government and NHS need to do to invest in care. We invite you to follow our campaign via #BGSInvestInCare @GeriSoc and share these important messages. |
- Almost 12 million people in the UK are of pensionable age and this is projected to rise to over 15 million by 2045. Health and social care systems must prepare for rapid growth of their largest user group.
(Source: Office for National Statistics)
- The number of people aged over 85 in the UK will almost double by 2045. Governments must plan now to meet the physical, mental and social care needs of the oldest old.
(Source: Office for National Statistics)
- 43% of consultant geriatricians in the UK are due to retire in the next ten years. Investment in the geriatric medicine and wider workforce caring for older people is overdue and essential.
(Source: Royal College of Physicians London)
- People aged 65 and over account for 40% of all admissions to hospital. Funding community services for older people can significantly reduce emergency hospital admissions and help NHS backlogs.
(Source: Hospital Episode Statistics, NHS Digital)
- Around 10% of people aged 65 and over and a quarter to a half of those aged over 85 live with frailty. Frailty costs the UK healthcare systems £5.8 billion per year. Frailty can be slowed or reversed with the right prevention and care, improving quality of life and saving money.
(Sources: Clegg, et al [2013]; Han, et al [2019])
- 30% of people over 65 and 50% of people over 80 will fall at least once a year. Falls cost the NHS more than £2.3billion a year. Investment in community falls prevention and response services improves quality of life for older people and saves the NHS money.
(Source: NICE)
- 15% of older people being discharged from hospital are readmitted within 28 days. Investing in coordinated discharge, intermediate care and community rehabilitation services saves the NHS money and improves lives of patients and families.
(Source: Vernon, et al [2019])
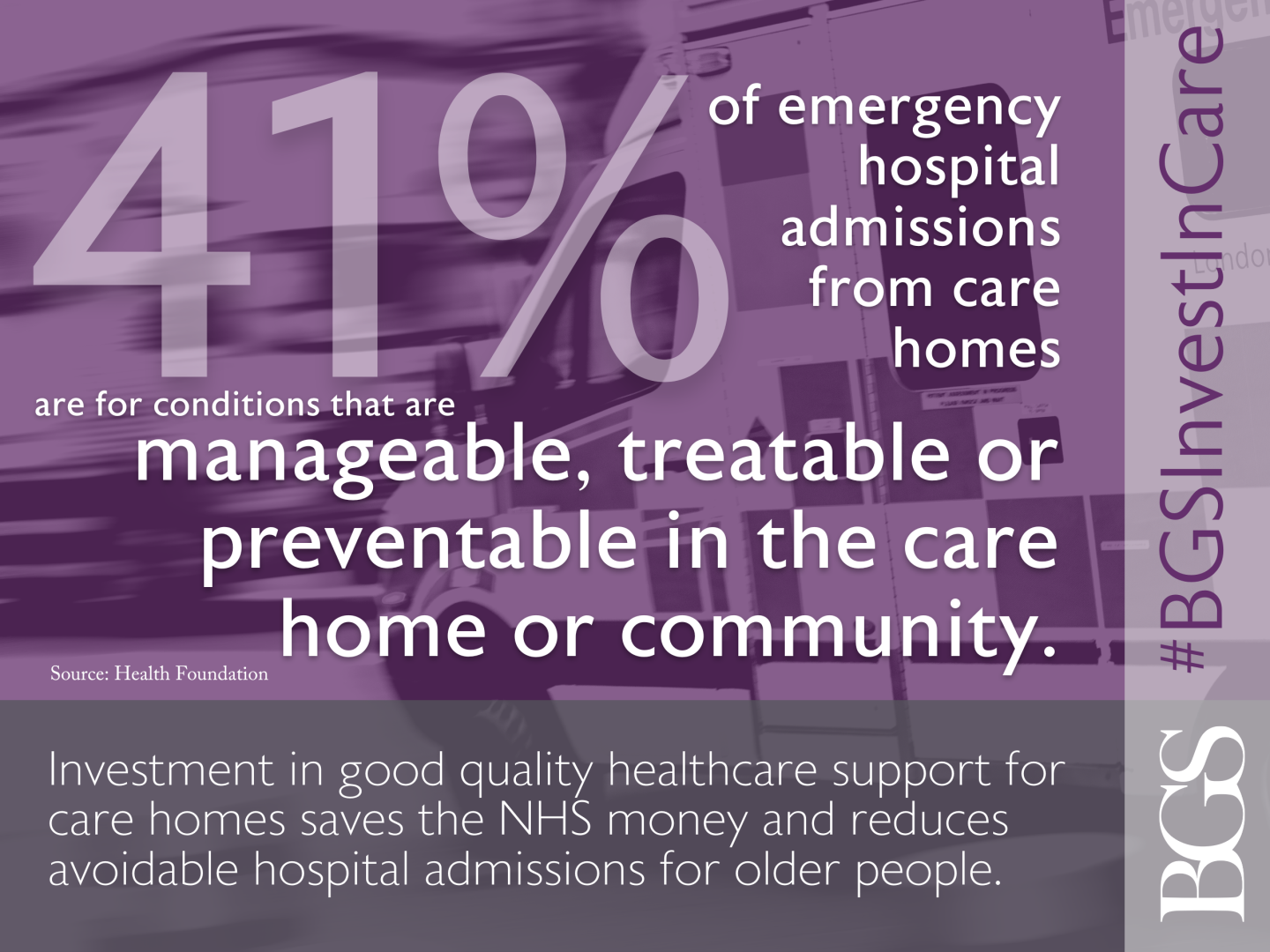
- 41% of emergency hospital admissions from care homes are for conditions that are manageable, treatable or preventable in the care home or community. Investment in good quality healthcare support for care homes saves the NHS money and reduces avoidable hospital admissions for older people.
(Source: Health Foundation)