Simon Conroy is a geriatrician at University Hospitals of Leicester and an honorary professor at the university. His research has focused on frailty, recognising its variation among older people and the need to personalise their care. He will be speaking at the upcoming BGS Autumn Virtual Meeting which is being held from 25 to 27 November 2020. He tweets @GERED_DOC
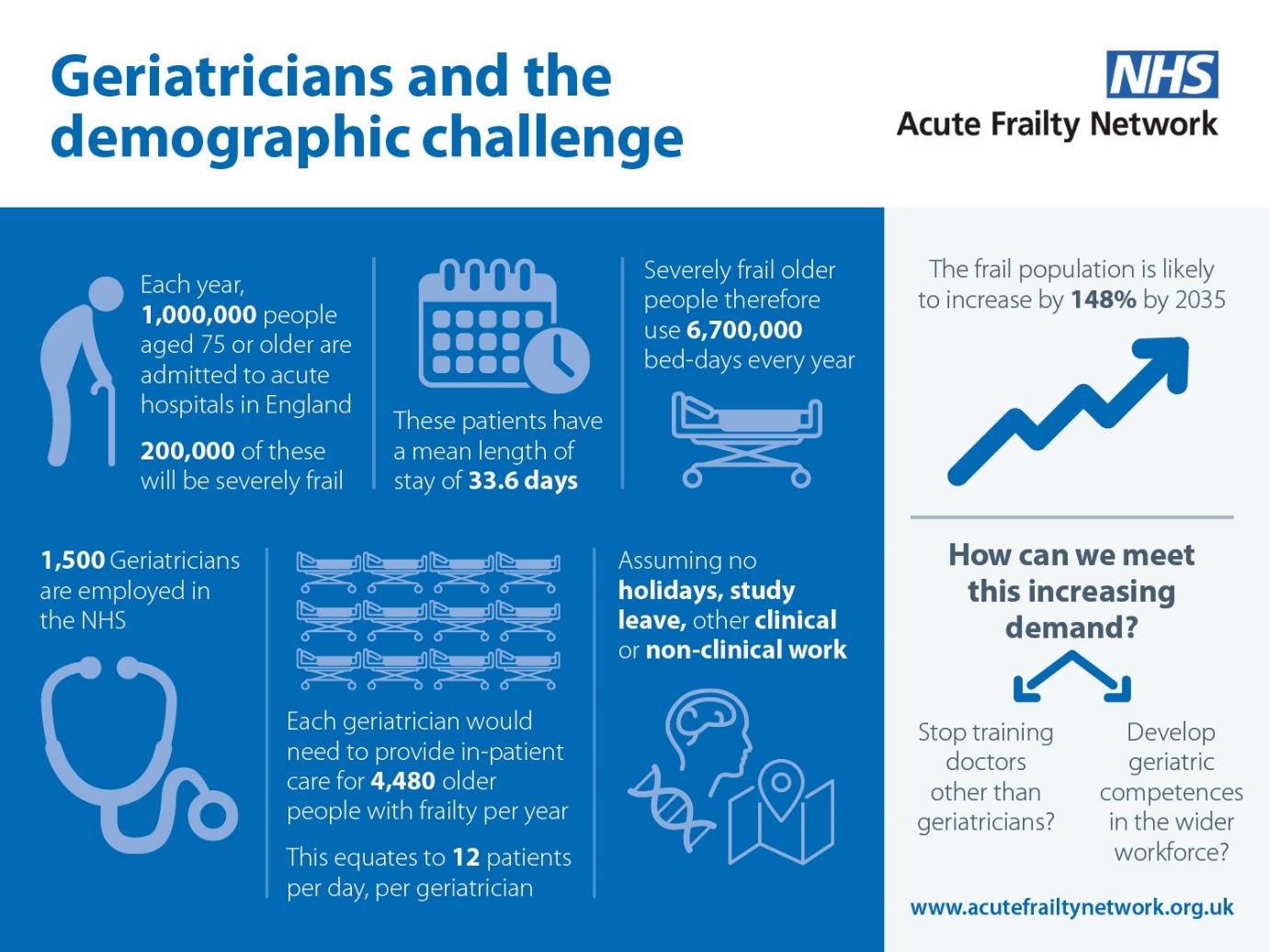
How do we achieve this Holy Grail? Robust evidence shows the benefits of Comprehensive Geriatric Assessment (CGA)1 for older people in acute settings, but how do we deliver this at the scale that is required? If you do the maths, it can’t be all about geriatricians (click here to see Figure 1), yet success in engaging non-geriatricians in delivering CGA remains somewhat elusive2.
There are a number of efforts underway to try and deliver CGA across many important pathways: Geriatric Emergency Medicine, Perioperative care of Older People, and many other support and/or liaison services for different settings. But most of these are geriatrician-dependant, which as Figure 1 suggests, has its limits as a long term strategy.
An alternative approach is to consider the essential ingredients in the CGA mix. These will include structures, such as adequate multidisciplinary staff or mechanisms to capture frailty at scale such as electronic frailty indices3 4, but also processes – regular team meetings, clear coordination and communication focusing upon patient-centred outcomes. Perhaps key are the clinical competencies that the geriatrician or frailty team bring to the care of older people, such as delirium management. These competencies, at least in theory, can be codified, taught/trained and transferred. A nice idea, but does it work in practice? Let me give you one example…
The Specialised Clinical Frailty Network (SCFN) is a clinically-led quality improvement collaborative, which supports specialised healthcare teams to improve the way care and treatment is tailored to the needs and preferences of individuals living with frailty. It has been working with specialised teams to explore how frailty assessment and management can best be integrated into specialised service pathways.
Wave One of the programme launched in September 2018, with 14 teams across 13 trusts, looking at Renal services, Transcatheter aortic valve implantation (TAVI) and Chemotherapy. The second Wave started in Feb 2019, with 14 teams from 11 sites looking at Spinal Surgery, Neurosurgery and Adult Critical Care. All of these sites were following the programme for six months, however we also worked with three extension sites from Wave One to explore the benefits of a longer programme of support instead. Wave Three sites launched in November 2019 looking at Cardiac Surgery, Cancer Surgery and Vascular Services, with a ten-month programme. Wave Four, looking at the same service areas, launches in October 2020.
There are case studies published on the SCFN website www.scfn.org.uk and an SCFN Toolkit which can be found here, aimed at anyone involved in the design or delivery of specialised services, working with older people with frailty. There are also a range of fully customisable packages to support frontline teams adopt the SCFN Toolkit, and to improve pathways in specialised services for older people living with frailty, available here.
If you are interested in hearing more about ongoing efforts to address Hospital Wide CGA, then please consider joining the session we will be holding at the BGS Autumn Meeting.
References
1. Ellis G, Gardner M, Tsiachristas A, et al. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database of Systematic Reviews 2017(9):CD006211. doi: 10.1002/14651858.CD006211.pub3.
2. Kocman D, Regen E, Phelps K, et al. Can comprehensive geriatric assessment be delivered without the need for geriatricians? A formative evaluation in two perioperative surgical settings. Age Ageing 2019 doi: 10.1093/ageing/afz025 [published Online First: 2019/03/28]
3. Clegg A, Bates C, Young J, et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing 2016;45(3):353-60. doi: 10.1093/ageing/afw039 [published Online First: 2016/03/06]
4. Gilbert T, Neuburger J, Kraindler J, et al. Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. The Lancet 2018;391(10132):1775-82. doi: 10.1016/S0140-6736(18)30668-8

