Jenni Burton is an Honorary Specialist Registrar (ST6) and NHS Education for Scotland/Chief Scientists Office Postdoctoral Clinical Lecturer in Geriatric Medicine at the University of Glasgow. She tweets @JenniKBurton
In case you missed it, June of this year saw the publication of ‘My Health, My Care, My Home – healthcare framework for adults living in care homes’. The framework was developed by Scottish Government working with care providers and representative bodies, health and social care practitioners, Health and Social Care Partnerships, policymakers and families and friends. Special thanks are due to Alyson Vale (Abbotsford Care) and the Fife Care Home Hub Team for their innovative resident engagement #HearMyVoice to ensure resident perspectives were also considered. I was fortunate to be involved in the reference and writing groups for the framework – an amazing opportunity to see how national guidance is developed and shaped.
It is important to highlight that Scotland does not have the Enhanced Health in Care Homes Framework, introduced in England in 2020. Thus there are different services and supports for residents across the country, with significant variation within and between regions. We know from the OPTIMAL study undertaken by Professor Claire Goodman and colleagues, that care homes receive reactive and inequitable support from NHS services. While there are examples of good practice and flourishing relationships, too often there are inconsistencies and barriers to residents accessing the same level of healthcare and support as those living elsewhere in the community. Care homes are individuals’ homes; residents live there as part of their community. Sadly, there are arbitrary divisions in service, denying access to those living in care homes, without a clear rationale or alternative accessible provision.
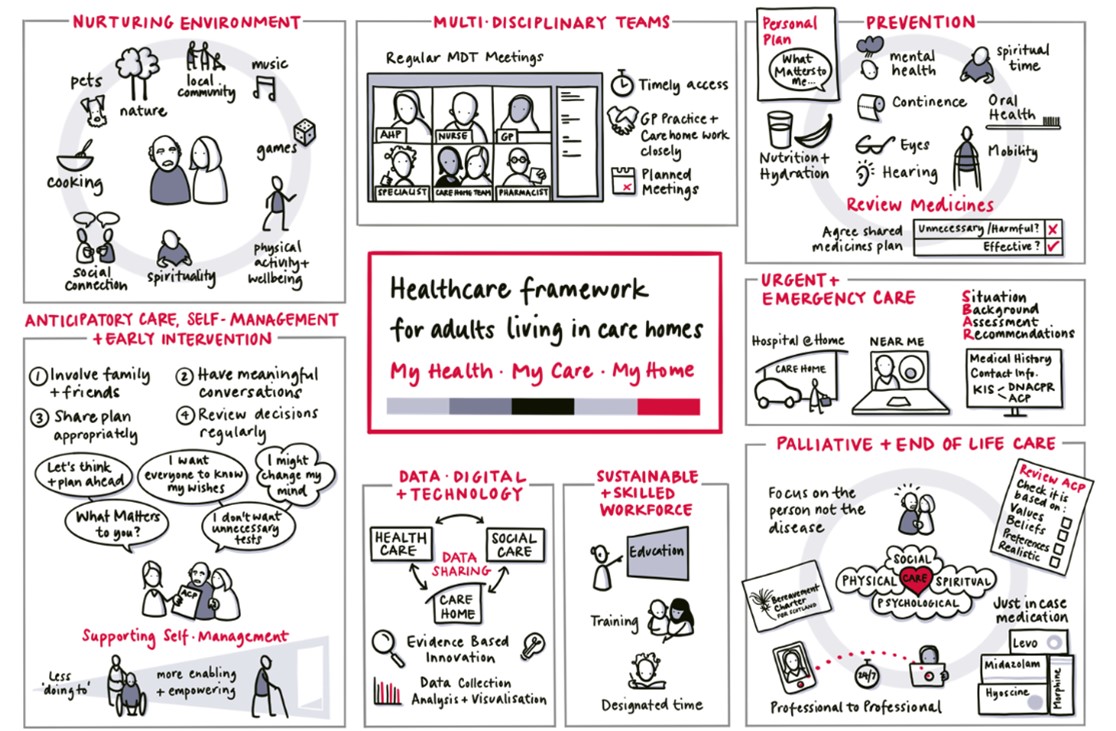
The new framework is based on six core elements: nurturing environment; the multidisciplinary team; prevention; anticipatory care, supporting self-management and early intervention; urgent and emergency care; palliative and end of life care, all of which are underpinned by a sustainable and skilled workforce and the effective use of data, digital and technology. Other enablers to the framework include Realistic Medicine (principles now embedded in NHS Scotland since their introduction in 2014) and ethical commissioning. The framework has been brought to life by the above fantastic graphic by Hazel White Design.
Following publication, an implementation plan will be developed to turn the aspirational framework into a reality. Critically, throughout the engagement work it was emphasised that change needed to be genuinely collaborative, working with the care home community, rather than ‘doing to’ them. Valuing their expertise, talent and skills is essential. Care home practice is specialist, highly skilled and distinct from care delivered in other settings.
With 78 recommendations, there is lots to consider, and each region will be starting from a different place in terms of their own landscape of services. National bodies have key roles to facilitate change, in addition to local plans developed by Health and Social Care Partnerships. However, I’m struck that as practitioners involved in clinical services, there are tangible practical things we can ALL do to make things better. Communication between acute care and care homes has tremendous scope for improvement – ensuring no care home resident leaves hospital without a copy of their discharge letter and medicines; ensuring that the letter is clear, avoids unnecessary abbreviations and that follow-up and changes are clearly described; ensuring the process in helpful to all our patients and their carers. Then there’s outpatient communication too, and how recommendations are shared with residents and staff.
NHS Highland Care Homes Team, led by Jaime Smith, have worked with their local care homes to develop ‘Home Safe’ – outlining the key actions for clinical teams to improve residents’ journey from acute to home. The aspects of Home Safe aren’t costly, but they are about ensuring effective discharge planning, good communication, professional respect and equipping homes to deliver seamless care by addressing the practical realities. Similarly, we developed a training video for acute and emergency care practitioners to raise awareness of the care home context and encourage professional-to-professional dialogue to support better decisions for individual residents.
At an organisational level, simple things like streamlining and improving visibility of key information such as the Care Home Information Portals/websites developed in Ayrshire & Arran and Lothian can help demystify clinical pathways. National digital infrastructure needs to change. Scotland is fortunate to have a single system for recording Anticipatory Care Plans, the Key Information Summary. However, while useable across primary, secondary and unscheduled care, care homes only have access if a copy is printed – missing valuable opportunities to contribute and update information about the individuals in their care. We still need to resolve our issues around routine data systems and the invisibility of the care home population, essential underpinnings of evaluation of the framework. However, better routine data must sit alongside measures of what matters to those living in care homes and those who support them.
The opportunities to share and develop good practice and provide equitable healthcare support for those living in care homes are there to be realised and this Framework will hopefully facilitate that change for homes across Scotland.