Current Structure
All newly qualified doctors will undertake a two year foundation training programme, consisting of four month blocks of medical training. This will be in a variety of hospital and community settings. Each year the trainee has to demonstrate progress against the foundation curriculum before they can be signed off. There are no specific examination requirements to pass the foundation programme, although for those trainees interested in pursuing a hospital based Medical career, the trainees are expected to pass the first part of the MRCP diploma before completing foundation training.
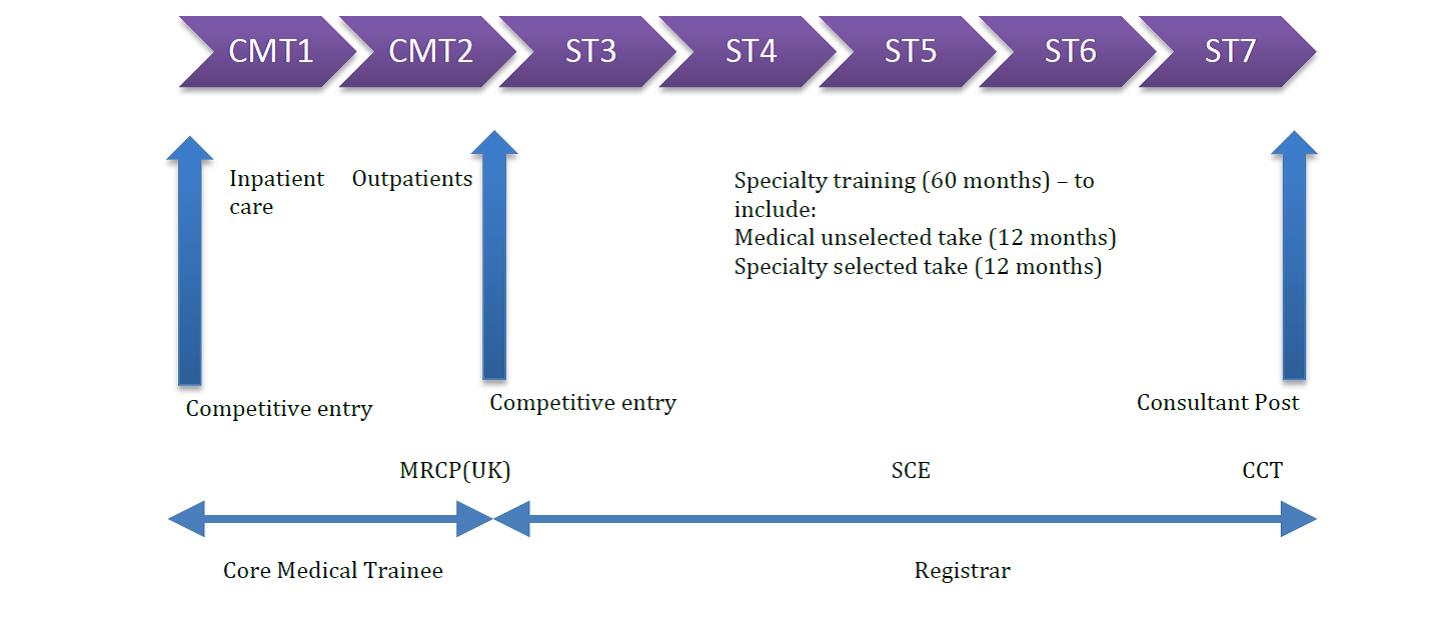
Hospital based Medical (as opposed to Surgical) trainees undertake a two year core medical training programme (CMT) during which time they are expected to pass the full MRCP diploma before going on to apply for specialty training (ST). Geriatric medicine trainees will end their five year training programme as recognised specialists in Geriatric Medicine and General Internal Medicine (GIM) – this is known as dual accreditation and gain entry onto the GMC’s specialist register by obtaining a Cerficate of Completion of Training (CCT). In order to complete the training programme they need to complete the Specialty Certificate Examination (SCE). For non-UK trained doctors, it is possible to get on to the specialist register by demonstrating equivalence of training – this route is often referred to as Article 14, or Certificate of Eligibility for Specialist Registration (CESR).
Planned Structure
Under the independent review of hospital medical training led by Prof Greenaway, there are significant changes proposed to the structure of medical training. There has been increasing concern about the relative lack of general training available to trainees, with some specialties such as dermatology and rheumatology having opted out of any general medical training during their higher
specialist training programmes. There was a relative shortage of middle grade doctors to staff the general medicine rotas on call, and a worry that in an age where doctors are expected to care for more patients with long term illnesses and multiple co-morbidities, a lot of specialty doctors were simply not being trained managing such patients.
Under the new proposals, trainees will still undergo two years of foundation training as they do currently.
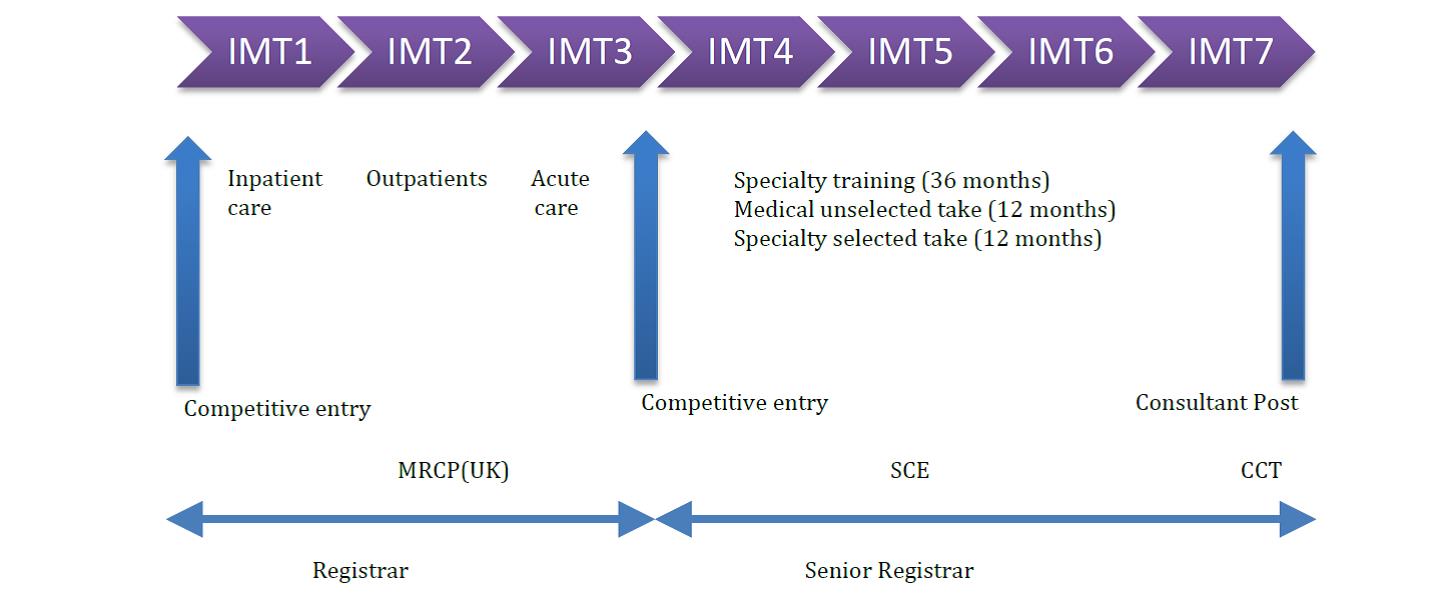
Core medical training has been replaced entirely with Internal Medicine training. Trainees will spend three years doing this during which time they are expected to pass the full MRCP diploma. One half of the first three years of internal medicine training should be spent in Geriatric Medicine training posts.
Trainees will then be able to apply for a four year higher specialist training programme, during which time they will still all be expected to take part in the medical on call rotas. Geriatric medicine trainees will end their five year training programme as recognised specialists in Geriatric Medicine and Internal Medicine (IM). The SCE will be retained. Trainees will be expected to obtain their CCT before getting a consultant post. CESR will be retained for non-UK trained doctors.
Additional terminology
Annual review of competence Progression (ARCP)
- All doctors occupying a specialty training post are required to undertake a yearly assessment of their progress (ARCP)
- Each ARCP is carried out by a small specialty based panel
- The ARCP will confirm the progress of the trainee through the training programme
- The ARCP is NOT an assessment in itself – the assessment will have been ongoing and carried out by the educational supervisor and colleagues in the working environment
Assessment: judging the trainee
- Formative: judging them to help/advise them
- Summative: judging them to decide on graduation
Appraisal: dialogue designed to support the trainee
Evaluation: measuring the education (quality, impact, structures)
Curriculum: GMC accredited account of programme expectations, outcomes etc
Outcomes: broadly drawn abilities expected of trainee
Competence: demonstrated ability to perform a task
Performance: consistent delivery of task
Evidence: document allowing a judgement, of outcomes or competence, by a 3rd party (panel)
Portfolio: compendium of such evidence
Decision Aid: document to direct panel on which ARCP outcome is justified by the available evidence
In summary an ARCP is the review of a trainee’s documented evidence of progress against their curriculum, resulting in a panel decision on the trainee’s further training.
ARCP Outcomes:
- 1 satisfactory, expected progress rate
- 2 specific competences still required (no extra time required in programme)
- 3 inadequate progress (extra time in programme)
- 4 released from the programme
- 5 inadequate evidence presented (may need more time in programme)
- 6 completed programme, CCT recommended
Penultimate year assessment (PYA)
- Trainee meets with representative of SAC external to their deanery
- Takes place 12-18 months before completion of training
- Aims to identify outstanding targets to ensure requirements of the curriculum are met in full
- Trainees will have 2 PYAs (Geriatric Medicine and Internal Medicine)