This publication outlines how to deliver proactive care against core components and key enablers, acting as a roadmap for implementing the NHS England framework and delivering proactive care services. This chapter sets explains what proactive care is, introducing the core components and key enablers for delivery.
Background
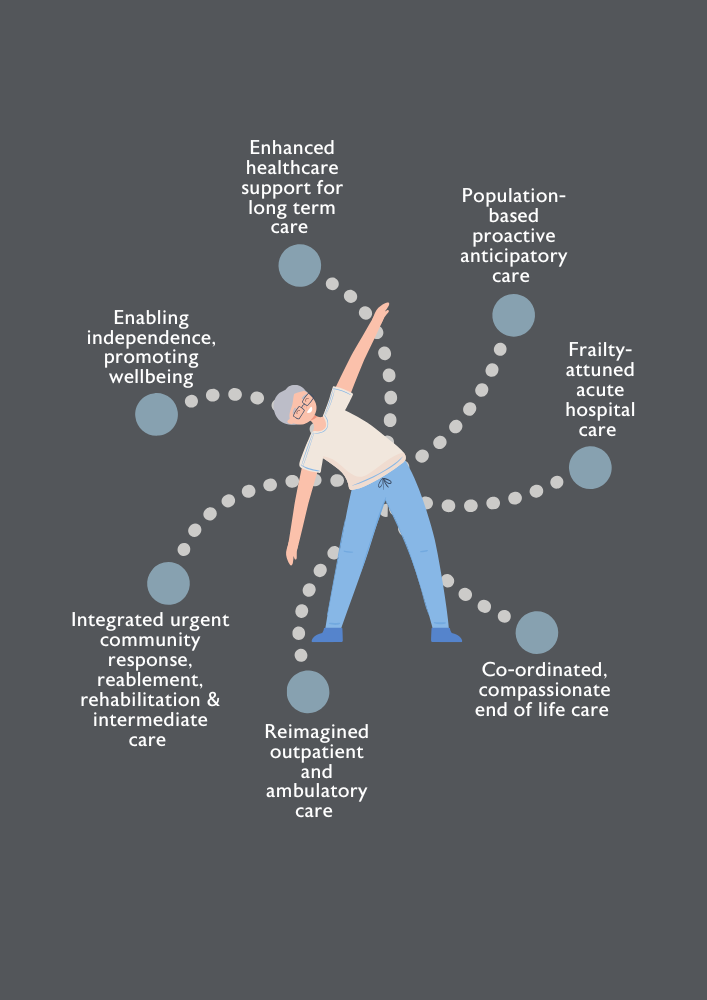
In June 2023, the British Geriatrics Society (BGS) published Joining the dots: A blueprint for preventing and managing frailty in older people.1 The publication acts as a blueprint to illustrate what good-quality age-attuned integrated care for older people looks like and makes the case for investing in services that prevent and manage frailty in older people. The blueprint sets out seven touchpoints of care that should be available to older people and makes 12 system recommendations. One of these vital touchpoints is “population-based proactive anticipatory care” which highlights the importance of care that targets people at risk of poor health and social outcomes to offer tailored support to stay healthier for longer.
This publication will explore the touchpoint in further depth, specifically focusing on proactive care aimed at older individuals with moderate or severe frailty receiving care in primary and community settings. This expands on NHS England’s Proactive care: providing care and support to people living at home with moderate and severe frailty,2 which is one of the three workstreams of the Ageing Well programme as published in the NHS Long Term Plan in 2019.5 Mapped onto NHS England’s five core components and three enablers of proactive care, this document acts as a roadmap on delivering proactive care for older people with frailty. It follows on from BGS’s Be proactive: Evidence supporting proactive care for older people with frailty, which outlines the evidence base for proactive care.3 It is hoped that those designing proactive care services will use all three documents in both making the business case for proactive care and delivering it.
How was this publication developed?
This publication was developed by members of the BGS’s Community and Primary Care Group (CPCG). It was informed by three workshops with a Professional Advisory Board consisting of 21 healthcare professionals from a range of healthcare backgrounds and locations, held between March – May 2024. The workshops focussed on the benefits of proactive care approaches, barriers and enablers to the implementation of proactive care services, approaches to the identification of people with frailty, and how proactive care can be implemented into the wider health policy system.
Proactive care policy
In December 2023, NHS England published guidance on proactive care, outlining how it can be used to provide care and support for people living at home with moderate or severe frailty.2 The guidance builds on previous reports calling for a transition to proactive care for patients living with frailty in the community. This includes the Fuller Stocktake, which calls for a healthcare system that better anticipates and manages the needs of individuals with frailty through more integrated, proactive, and community-centred care.6 Outlined methods include the identification of patients with frailty and targeted delivery of interventions to prevent crisis, integrated care to support improved transitions of care, place-based models of care, and investment in Multidisciplinary Teams (MDTs). Similarly, the England Chief Medical Officer’s annual report 2023: health in an ageing society highlights the importance of maximising the independence of older people through the promotion of healthy ageing.7 This will prevent and delay the onset of frailty in older people and in turn reduce hospital admissions, which has increased over the last 15 years.8 This requires investment and a re-focus on care delivered within community and public health settings.
Whilst England is the only nation in the UK with a national proactive care framework, health and social care policy in Scotland, Wales, and Northern Ireland also features proactive care. In Scotland, the 2017 Health and Social Care Standards: My Support, My Life emphasised the importance of early identification and support for individuals with frailty.9 In 2024, the Ageing and Frailty draft standards for the care of older people were published with 11 standards, which included the proactive identification of people living with frailty.10 In Wales, the Older people and people living with frailty: integrated quality statement published in January 2024 called for integrated community focused care to provide proactive, urgent and crisis care management in the community. 11 This will involve proactive identification and management of frailty as a long-term condition to prevent, delay, reverse or slow down its progression. Finally, in Northern Ireland one of the four core priorities of the Northern Ireland frailty network is the early identification of frailty to deliver more efficacious management of frailty.12
The NHS England proactive care guidance is a crucial starting point for Integrated care Boards (ICBs) and provider organisations designing and implementing proactive care.2 The guidance identifies five core components of the proactive care approach and three enablers:
Core components
- Identifying the target cohort for whom there is the greatest potential impact on health and system outcomes.
- Carrying out holistic assessments, such as a Comprehensive Geriatric Assessment
- Developing a personalised care and support plan.
- Delivering Co-ordinated multi-professional interventions to address the person’s range of needs.
- Providing a clear plan for continuity of care, including an agreed schedule of follow-ups.
Key enablers
- Flexible workforce.
- Shared care record.
- Clear accountability and shared decision-making.
The NHS England guidance identifies the importance of proactive care but lacks specific details about how to implement proactive care services in local areas and at larger scales. Whilst it is a key starting point, the BGS is disappointed in the absence of funding for the programme compared to what was originally proposed.13 This document aims to build on the NHS England guidance through outlining how to deliver the five core components and three key enablers of proactive care.
Audience
Supporting primary and community care services to deliver proactive care programmes is in the interest of the wider health system. However, given the broad range of challenges, coordinated action is required incorporating the whole multidisciplinary team. This document aims to be a useful guide for healthcare professionals, clinical leaders, commissioners, and system designers wishing to set up proactive care services within primary and community care settings in their local areas. It also provides commissioners and policy makers with key recommendations on how to set these services up on a larger scale. Whilst we use the NHS England guidance as a starting point, the principles outlined in this document can be implemented across all four nations.

What is proactive care?
Defining proactive care
Frailty is not an inevitable part of ageing, and proactive care aims to reduce or delay negative health outcomes through targeting those at risk of frailty and tailoring health interventions to support them live well for longer. It aims to delay the onset of health deterioration, maintain independent living, and reduce avoidable periods of ill health, thereby reducing unplanned care.2 Most healthcare interactions for older people with frailty take place in primary care, and it is therefore a crucial setting for proactive care services to be implemented. 14 Within primary and community care, there is an increasing focus upon proactive models of care to identify, assess and manage older people with frailty to mitigate the negative impacts of frailty on individuals and healthcare systems.15 Importantly, this transforms care from being reactive, fragmented, and episodic to personalised, community-based, and coordinated.16
Benefits of proactive care
There is significant scope for proactive care delivery within primary and community care systems to improve patient-centred outcomes and system-centred outcomes. Benefits to patients include improved quality of life, reduction in loneliness/isolation, reduction in carer burden, and the maintenance of independence.17 In turn, this can lead to wider healthcare system benefits, such as reduced hospital admissions and re-admissions.
Target cohort for proactive care
The NHS England guidance on proactive care focuses on people with moderate to severe frailty living in their own homes, excluding those with mild frailty. Most healthcare professionals working with older people will be caring for those with moderate to severe frailty, and therefore, our focus will also be on this cohort. The BGS recognises the importance of targeting those with mild frailty and the biggest system impact may be had by targeting this cohort. However, due to the high number of older people with mild frailty, this will require a different preventative screening approach, focussing largely on public health interventions incorporating exercise, nutrition, and overall wellbeing.18
The evidence base
There are conflicting concepts around frailty, its measurement and its relationship to multiple long-term conditions, ageing and disability.19 Despite this, there is a broad consensus that the impact of frailty on individuals and care systems warrant a proactive inter-professional primary care approach to identification, assessment and management.20
There is evidence that proactive care programmes for patients with frailty are beneficial, with trials in the UK and Netherlands reporting reduced functional decline, improved quality of care, improved wellbeing, and improved quality of life.21-23 Individualised care planning, including medicines optimisation and regular review, has been identified as the intervention with the strongest evidence base for sustaining independence in older people in the community.24 Similarly, continuity of care has been identified as vital in proactive care service’s success and delivery.
Currently, the implementation of proactive care programmes is based on evidence-informed rather than evidence-based practice, which can prove challenging for commissioners. However, clinical research and quality improvement will lead to adjustments and redesign of proactive frailty interventions and help support the development of new knowledge and evidence for this patient group.25
The ability for different localities to implement proactive care programmes for patients with frailty is dependent on funding and workforce pressures. Despite this, current evidence highlights four key themes for the successful delivery of proactive care services. Firstly, the ability for a service to deliver Comprehensive Geriatric Assessment (CGA) is a priority. CGAs should provide patient centred assessments to identify symptoms or functional decline, including screening tools such as the PRISMA-7 questionnaire, Gait-Speed (four-metre walk), and timed-up-and-go tests.26 Secondly, the identification of a clearly defined group of patients is pertinent. Depending on the size of the proactive care programme, this can range from annual screenings with frailty tools, to the identification of individuals with a high number of primary care contacts, home visits, medications, or medical conditions.27 The type of intervention needs to be tailored depending on size, resources, and aims. Thirdly, it is important that proactive care programmes are resourced sufficiently.28,29 While there appears to be general support for proactive care programmes from GPs, there are concerns that under resourced interventions will lead to high workloads without benefits.28,29 Finally, integration with the broader health and social care system is beneficial to support wider components of care, such as nutrition, social interaction, and exercise. Examples include linking to social prescribers, referrals to day centres or community hubs, and integration with the third sector.
BGS's Be proactive: Evidence supporting proactive care for older people with frailty3 provides further information on the evidence base behind proactive care. This document outlines detailed evidence which was originally gathered to inform the NHS England guidance document and has been published with the approval of NHS England. Healthcare teams will be able to use this evidence to build business cases for proactive care services.


