This section of our blueprint describes the key touchpoints of care and support for older people across the system, from prevention through to end of life care. It describes the evidence-based approaches and interventions that are required to prevent and manage frailty across the continuum of care.
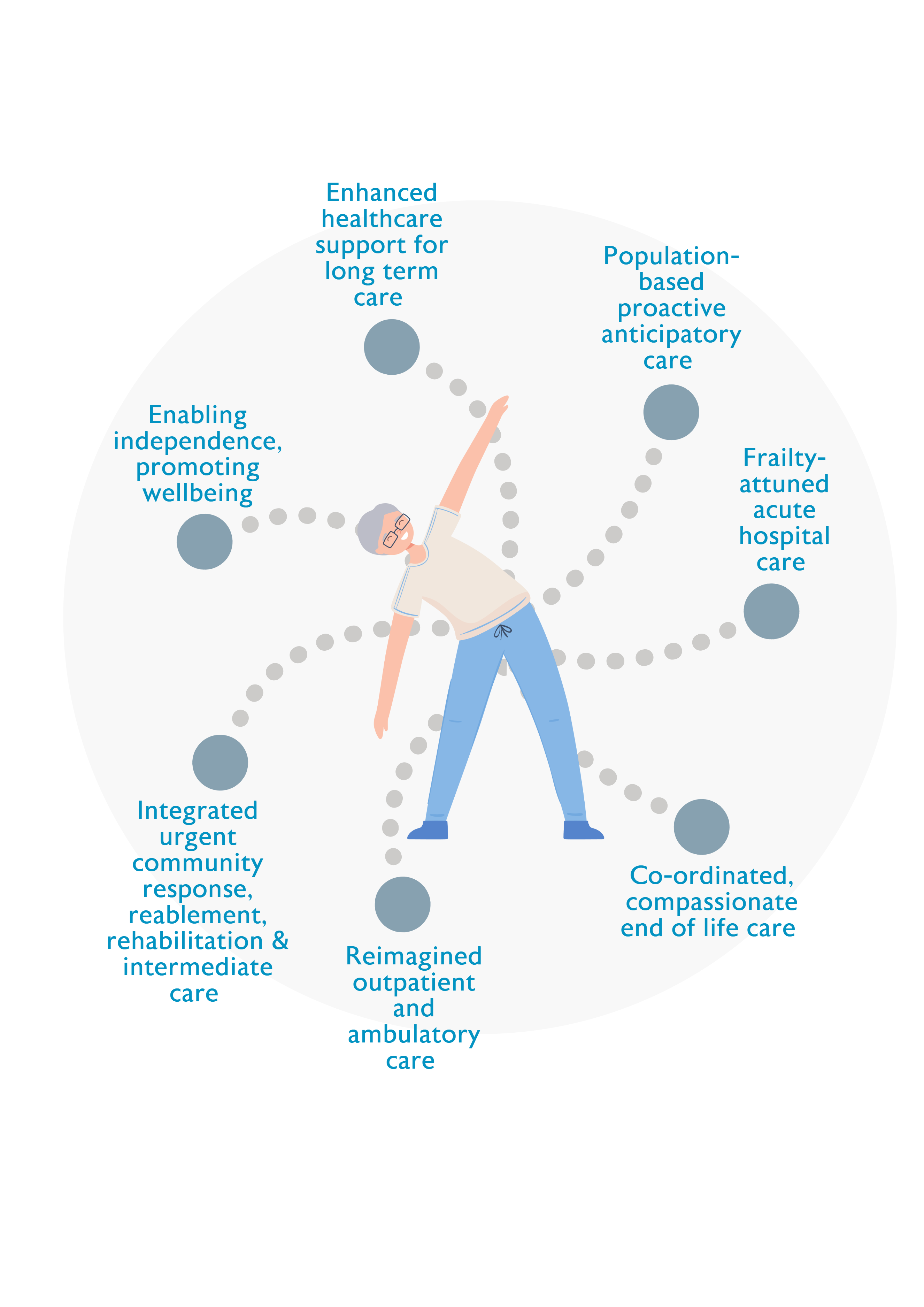
The evidence-based approaches and interventions that are required to prevent and manage frailty across the continuum of care are interdependent and mutually reinforcing and should be designed as ‘wrap around’ services that are available for all older people, wherever and whenever they are needed. Services that are designed around the needs of older people will reduce the number of people admitted to hospital as an emergency, promote early discharge home, and ensure that fewer people are readmitted to hospital or to long term care. This in turn improves outcomes for older people and reduces costs for the NHS and social care.
Enabling independence, promoting wellbeing
Case study
Make Movement Your Mission (MMYM), developed by the Later Life Training charity, broadcasts freely accessible 15 minute ‘movement snacks’ three times per day on Facebook (live and recorded) and YouTube. The key message, ‘sit less, move more’ applies to all ages and abilities. Participants (age 40 to 90+ at home and in care settings) include people with neurological or musculoskeletal conditions that need regular movement to slow progression or reduce symptoms. Participation and activity levels are promoted by support from the online instructor, Facebook messages pre and post live sessions, peer support, and self-motivation from noting improvements in balance and posture. Feedback indicates that the regular short movement snacks are felt to be achievable, provide a routine and offer opportunities to engage with others. In an independent evaluation, 90% of respondents said they moved more frequently and regularly every day; 53% reported better quality of life; and up to half reported improvements in activities of daily living (ADLs). Participants on waiting lists for joint replacement were kept mobile and had less pain.
Other examples
Mid & East Antrim Agewell Partnership (MEAAP), Ballymena, Larne & Carrickfergus, Northern Ireland
www.meaap.co.uk/impactagewell
Age Friendly Manchester
www.manchester.gov.uk/info/200091/life_over_50/8388/find_out_about_age_…
Other useful resources
- BGS Healthier for Longer (2019)
www.bgs.org.uk/healthierforlonger - World Guidelines on Falls Prevention and Management (2022)
https://academic.oup.com/ageing/article/51/9/afac205/6730755

Population-based proactive anticipatory care
Proactive anticipatory care targets people at risk of poor health and social outcomes in order to offer tailored support to stay well. Individuals at risk of poor outcomes are identified using validated population level screening tools combined with professional judgement.
Those with significant or escalating risk are offered a comprehensive multi-disciplinary assessment and appropriate interventions co-ordinated by a local multidisciplinary team of healthcare, social care and community or voluntary service partners working together. The older person and their carer or family will be involved in developing a personalised care plan based on their goals and preferences. Emerging evidence shows that the approach can improve care continuity and coordination and reduce emergency attendances. In the long term, the approach aims to reduce healthcare inequalities and improve system outcomes.
Case studies and examples
North Lanarkshire HSCP developed an innovative collaboration between the health/ social care locality team, primary/ secondary care professionals and a voluntary sector partner to provide person-centred, anticipatory care for older adults with escalating levels of frailty and high risk of deterioration in the community. Initially the holistic frailty assessment was completed by a Health Visitor band 5. Covid-19 prompted an innovative partnership with Equals Advocacy (EA) who already had a track record in facilitating Anticipatory Care Planning (ACP). With initial support EA workers were able to undertake home frailty assessment focussed on ‘What Matters to Me’. Moving to a virtual MDT format has saved time and travel. Attendees include Advocacy Worker, Primary Care Senior Decision maker, Older People’s Community Mental Health Team, Care at Home Manager, Advanced Clinical Services Pharmacist, Frailty Specialist, Community Nursing and Community Rehabilitation Team Lead. The MDT developed six standard interventions for all and additional tailored interventions depending on need. The Advanced Clinical Services Pharmacist within the MDT has resulted in improved pharmaceutical outcomes and reduced inappropriate polypharmacy. A formative evaluation is underway.
Other examples
Proactive Telecare provided by Delta CONNECT, West Wales
www.deltawellbeing.org.uk/delta-connect
Other useful resources
- NHS England Anticipatory Care operating model and intervention framework
https://future.nhs.uk/CommunityHealthServices/groupHome (login required) - BGS Community Case Studies
www.bgs.org.uk/resources/community-geriatrics-video-case-presentations - BGS Anticipatory Care Blog Series
www.bgs.org.uk/AntCare - PrescQIPP Polypharmacy and Deprescribing Polypharmacy and deprescribing
PrescQIPP C.I.C - RPS Polypharmacy Getting our medicines right 2019 Polypharmacy: Getting our medicines right (rpharms.com).

Integrated urgent community response, reablement, rehabilitation and intermediate care
Many older people who experience an acute illness or decompensation of a frailty syndrome prefer to receive healthcare at home or closer to home.
Case studies and examples
The Western Health and Social Care Trust in Northern Ireland established a Hospital at Home (H@H) service in rural County Fermanagh. Initially restricted to four Care Homes, the service now supports older people at home across the County. Current staffing is a less-than-fulltime Lead Consultant, two WTE Specialty doctors, ten WTE Nurses, three WTE Health Care Assistants and one WTE Pharmacist. The service provides acute care for between four and six patients per day seven days per week with over 97% of patients assessed within two hours of referral. 82% were identified by GP or ambulance colleagues. The remainder were early facilitated discharges from the acute hospital. For 229 patients managed between December 2020 and May 2022, median length of stay was 5.5 days. There were no complaints or reports of adverse incidents. Any deaths during or within 30 days of H@H care are discussed at the Acute Hospital’s Morbidity and Mortality meeting, to support assurance and learning and to increase the visibility of H@H to acute clinicians. There is a need to build productive alliances with primary care and with the local Ambulance service to enhance acute care options for older patients. Through linking with Ambulatory and Geriatric Clinic services, generalist and palliative care services, and specialist community respiratory and cardiac services the team aim to build a productive, bureaucratically-light suite of options for acute care and follow-up to best meet the needs of older people in the local community.
Other examples
The Frailty Support Team in the New Forest69
www.bgs.org.uk/resources/community-geriatrics-video-case-presentations
Heathlands Intermediate Care Unit
www.fhft.nhs.uk/news/new-unit-praised-by-patients
Other useful resources
- BGS Community Case Presentations:
www.bgs.org.uk/resources/community-geriatrics-video-case-presentations
- Midlothian’s Hospital at Home story
https://sharingandlearningonline.wordpress.com/hospital-at-home

Age-attuned acute hospital care
Older people with frailty account for a significant amount of hospital admissions and often have poor experiences and outcomes from urgent care.70 Many older people with frailty admitted to hospital as an emergency could be fit to return home on the same day if they were assessed, diagnosed and treated swiftly on arrival at hospital.
- Acute care at the front door - Emergency medicine specialists and geriatricians worked together to develop shared competencies in frailty and emergency care to enable early holistic assessment of older people in urgent care in order to alter their care trajectories and to improve experience and outcomes.74 The work was supported by a common vision, trusted relationships and joint education and training between the two specialties.
- Acute frailty services routinely and systematically identify frailty in people attending Urgent and Emergency Care services. They consider the personalised needs, including the level of frailty and degree of illness, and are supported by clear reliable hospital-wide pathways aligned to the level of frailty identified.
- Same day emergency care (SDEC) can allow specialist senior clinicians to care for patients on the day they arrive at hospital as an alternative to admission, removing delays for patients requiring investigation and/or treatment. Patients with conditions such as frailty can be assessed, diagnosed and treated without being admitted to a ward and, if clinically appropriate, return home on the same day. Some episodes of care may require follow-up for review and/or treatment to eliminate the need of overnight admission. SDEC can provide an opportunity to embed the acute frailty pathway within an Acute Trust. This may be particularly effective when linked with integrated frailty services. These services include integrated primary and acute care models (GPs working in hospital or interface geriatricians working in A&E departments) or community models with neighbourhood health and social care teams wrapped around GP practices.
- Orthogeriatric services and Perioperative medicine for Older People undergoing Surgery (POPS) - Increasing numbers of older people undergo emergency or elective surgery.75 Clinician-reported, patient-reported and process-related outcomes are poorer in older surgical patients compared to younger people.76 Clinical and cost effectiveness data show that older surgical patients who receive CGA-based perioperative care have better outcomes and experience in both emergency and elective surgical settings.77 However, implementation of such services remains patchy78 as evidenced in national audits of falls and fragility fractures. A new guideline79 coordinated by the Centre for Perioperative Care and the BGS covers all aspects of perioperative care relevant to adults with frailty undergoing elective and emergency surgery.
- Dementia management – 944,000 people in the UK are living with a diagnosis of dementia and this is projected to increase to 1.6 million people by 2050.80 The cost of dementia to the economy is projected to nearly double by 2050, from £25billion in 2021 to £47billion.81 A quarter of hospital beds are occupied by older people who have dementia and the majority of people who have dementia have at least one or two other long-term conditions – only 12% of people with dementia have no co-morbidities.82 Older people with dementia are at higher risk of poor health outcomes when they present at urgent care settings and may spend longer in emergency departments. Patients with dementia may have vague symptoms or be unable to report their symptoms, resulting in higher rates of burdensome or invasive testing.83 Further advice on managing dementia in an urgent care setting can be found in the Silver Book II.
- Delirium management – Poorly identified, assessed and managed delirium not only extends length of stay but can cause significant distress for patients, carers and staff. The Frimley ICS introduced a specific delirium pathway that runs for up to 12 weeks, recognising that delirium takes time to resolve. Inpatients with possible delirium are referred to the acute frailty team who undertake a comprehensive geriatric assessment and suggest a management plan. If the patient’s discharge care needs have increased as a result of delirium, increased funding is available and continues until review by an integrated care team comprising mental health/GP/community matrons and social care. The team review patients at six and 12 weeks and assess if the delirium has resolved, or if they need to stay on the pathway. If a new cognitive baseline has been reached care is then funded through the usual arrangements. Further advice on managing delirium can be found in the BGS Delirium Hub.
- Reducing deconditioning – The University Hospitals of North Midlands NHS Trust began a ‘Sit up, get dressed, keep moving’ campaign to raise awareness of how to prevent deconditioning. This campaign encourages older people in hospital to be active and supports healthcare professionals to help their patients to remain active. This supports older people’s recovery, reducing the chances of them being readmitted to hospital in the days following discharge. Their work is complemented by an international campaign to enrich the last 1000 days for older people with frailty. #endPJparalysis84 https://improvement.nhs.uk/resources/our-endpjparalysis-journey
- Hospital discharge and D2A pathways – The NHS England National Health and Social Care Discharge Taskforce85 identified 10 best practice initiatives that should be implemented in every trust and system to improve discharge and flow. The recommended approach includes framing delays to discharge as a potential harm event. The best practice initiatives are similar to the Home First principles and actions in Scotland’s Discharge without Delay programme.86 Both programmes promote Discharge to Assess87 at home or in the community and acknowledge the need to ensure capacity for intermediate care and rehabilitation to optimise recovery after discharge to improve outcomes for people and reduce further demand for services.
Other useful resources
- Silver Book II
www.bgs.org.uk/resources/resource-series/silver-book-ii - Acute Frailty Network
www.acutefrailtynetwork.org.uk - Scottish Care of Older People (SCoOP) Project
www.bgs.org.uk/resources/scottish-care-of-older-people-scoop-project - Right time, right place: Urgent community-based care for older people
www.bgs.org.uk/righttimerightplace

Reimagined outpatient and ambulatory care
The need to adjust the traditional outpatient model for older people is increasingly pressing. There is growing evidence for personalised patient-initiated follow up, albeit more studies are needed to assess outcomes for older people.
- Decreased need for transport to attend clinic; the home environment is more comfortable.
- Decreased requirement to wait in hospital waiting rooms/corridors for appointments.
- Increased opportunities for family members or translators to ‘dial in’ and participate.
- Increased opportunities for multi-professional input in a single appointment.
- Opportunities for remote monitoring to allow early recognition of physical problems, or ongoing assessment of existing issues in real time.
- Decreased numbers of ‘Did Not Attend (DNA)’ due to issues with hospital transportation systems.
- Increased efficiency with a greater number of telephone appointments feasible.
- Decreased carbon footprint of outpatients with fewer in-person attendances.
Case studies and examples
Hull and East Riding provides a hybrid proactive / reactive Community Frailty Anticipatory Care Model in an area with high levels of health inequalities and deprivation. A specialist Frailty MDT includes Consultant Community Geriatricians, GPs with Extended Roles (GPwER) in Frailty, Advanced Nurse Practitioner, Pharmacist, Pharmacy technician, Social worker, OT and PT, Carers Support service, Clinical Support Workers and Chaplain. The team offer CGA as a one stop ambulatory care model at the Jean Bishop Integrated Care Centre, with dedicated ambulance transport support. A virtual CGA is also delivered weekly for those living in rural / remote locations. Observed benefits include good Patient Reported Outcome Measures (PROMs) for individuals, a reduction in use of unscheduled primary and secondary care, high levels of staff satisfaction, innovative workforce development and successful recruitment into a historically under resourced service area and location.
The Jean Bishop Integrated Care Centre
https://www.youtube.com/watch?v=zFhjHx0s9q0
Other examples
Lancashire and South Cumbria Health and Care partnership’s Hot clinic:
https://www.flowcoaching.academy/case-studies
Dwyfor Primary Care Cluster
www.rcplondon.ac.uk/projects/outputs/outpatients-future-adding-value-th…
Virtual geriatric perioperative care clinic, North Bristol NHS Trust
Age and Ageing 2021;50:1391–1396 https://doi.org/10.1093/ageing/afab066
Other useful resources
- Royal College of Physicians (RCP) - Outpatients: the future – adding value through sustainability
www.rcplondon.ac.uk/projects/outputs/outpatients-future-adding-value-th…

Enhanced healthcare support for long term care at home and in care homes
Care homes are home to around 400,000 older people with frailty.89 The average care home resident is 85 years old, has six medical diagnoses and takes eight medications.90 The majority of residents have high care needs and are in the last two years of life.
Case studies and examples
Rushcliffe in suburban Nottinghamshire has a 1:1 relationship between GPs and care homes, with GPs supporting quality improvement and co-ordination of care in addition to routine primary care. The enhanced service specification comprises regular scheduled visits to care homes and proactive review of medications and care plans accompanied by community nurses who offer peer support, training, signposting and review of direct referral pathways to community services. Regular meetings between NHS and care home staff build relationships and a care home managers network is facilitated by Age UK. The service achieved a 40% reduction in emergency admissions to hospital from care homes, 50% reduction in avoidable admissions for ambulatory care sensitive conditions, and a 43% reduction in Emergency Department attendances.
Nottingham City Care Home Vanguard established a 1:1 relationship between GPs and care homes, with contractual specification for regular visits and scheduled proactive review of medications. A dedicated Care Homes Nursing Team provided all community nursing input in to care homes in the locality, including proactive assessment and case management of all new residents. The service established specific MDTs to work with care homes around dementia care and falls prevention, streamlining referral pathways to minimise bureaucracy and delays. Care home staff and managers were actively involved in service design and service-level decisions about care homes and in structured training and forums for staff and managers. The service achieved 34% reductions in emergency admissions and 39% reduction in potentially avoidable admissions, contributing to a trend towards cost savings. Staff, resident and carer satisfaction with care delivery was higher than for comparator sites.
Other examples
South Sefton Care Home Improvement Project
www.southseftonccg.nhs.uk/get-informed/latest-news/ccg-scheme-to-improv…
Tameside and Glossop Integrated Care NHS Foundation Trust’s digital hub
https://tamesideandglossopicft.nhs.uk/services/digital-health-services
Other useful resources
- British Geriatrics Society. Ambitions for change: improving healthcare in care homes
www.bgs.org.uk/ambitions-for-change - The impact of providing enhanced support for care home residents in Rushcliffe - The Health Foundation
www.health.org.uk/publications/the-impact-of-providing-enhanced-support… - Reducing hospital admissions in older care home residents: a 4-year evaluation of the care home innovation Programme (CHIP). BMC Health Serv Res 2020;20:94. doi:10.1186/s12913-020-4945-9

Co-ordinated, compassionate end of life care
End of life care for older adults living with multiple health problems and frailty is different from dying with a single disease. The range of trajectories of decline includes sudden death, slow progressive deterioration (such as in advanced dementia), catastrophic events (such as stroke or hip fracture), and periods of prolonged uncertainty associated with fluctuating episodes of acute illness associated with delirium or functional decompensation.95
Case studies
The Geripall service in Sutton, Surrey aimed to improve the clinical pathway for people with advanced frailty (CFS 7-9) approaching the end of their lives. To be included, patients must be registered with a Sutton GP, have late-stage dementia or other neurodegenerative conditions, be at risk of recurrent unplanned admissions and have no specialist palliative care needs. Referrals are accepted from: Acute Frailty Unit and staff, other medical and surgical areas, Rapid Response Team in community, or social services.
A frailty consultant provides advice as and when required and a Geri GP works three sessions supporting a Band 7 nurse. The nurse is responsible for:
- Communicating with patients, family, carers, ward staff and discharge team, convening a family conference if required
- Reviewing medication, prescribing “just in case” medicines, and updating records accordingly
- Advance Care Planning
- Fast Track referral for CHC funding, and follow up in the community including by phone and through visits, referring to appropriate agencies as needed
- Communicating with the patient’s GP and other agencies as required.
- Service outcomes are reduced length of stay, reduced readmission at end of life, improved carer and patient involvement and experience of care.
Other examples
The Bromley Care Coordination Team
www.stchristophers.org.uk/leaflet/bromley-care-coordination-at-st-chris…
Other useful resources
- BGS End of life Care in Frailty Guidance
www.bgs.org.uk/resources/resource-series/end-of-life-care-in-frailty - Ambitions Framework
www.england.nhs.uk/wp-content/uploads/2022/02/ambitions-for-palliative-… - NHS England Specialist palliative and end of life care services: Adult service specification January 2023
www.england.nhs.uk/publication/service-specifications-for-palliative-an…
