Frailty is a pressing issue at all levels of healthcare.22
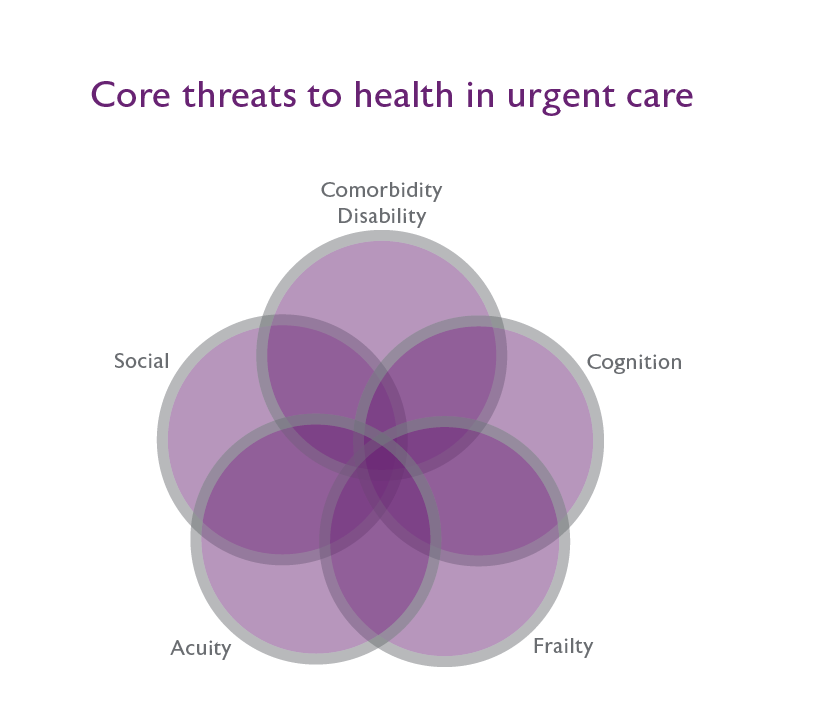
First, the essence of frailty is misunderstood. The background risk (the degree of frailty) goes unacknowledged, much less identified and addressed. Acknowledged or not, frailty, and its typical accompaniments of multiple, interacting medical and social problems that produce varying grades of disability, play essential roles in the delivery and outcomes of care. That the complexity of frailty mostly goes unrecognised, is as an unintended consequence of healthcare’s tremendous success from ever greater focus, manifested as diagnosis-based, deeply ingrained, hard-won specialist expertise.
Second, this privileging of a narrow, disease-based focus means that, the idea of the whole person is often seen at best as an issue for other health care providers, and at worst as 'social considerations' not legitimately within the purview of whichever subspecialty is treating their problem. In consequence, how to mitigate the risk associated with frailty is not yet part of the skill sets on offer routinely and at scale.
Third, and most important, especially in systems only coming late to recognising frailty - is that not only do we not routinely mitigate risk from frailty, but many routine health care practices unnecessarily increase it. For example, in the hospital setting it is common to see somewhat less than full vigilance in patients being able to sleep, to eat, to drink, to have intravenous fluid therapies that correspond to their age-related needs, to have pain treatment optimised and medications rationalised.
It is the system that must respond: this is not the work of a few people. Health care systems that have been successful in addressing these challenges – and no system yet can claim complete success - typically emphasise naming and staging frailty.23 Naming frailty without staging it runs the risk of having ‘frailism’ as the polite face of ageism. For example, the needs of people with mild frailty differ vastly from those who are very severely frail. For the former, the case can be made that what is most needed is better routine care. This includes an ability to respond to more than one problem at a time, to take a whole-person view of wellbeing and prevention24 and to improve the routines of hospital care. In contrast, people who are very severely frail – who spend much of their time in bed, with increasing dependence – typically need management suitable to people living in their last year of life.25 These competing needs are not easily reconciled in a single frailty pathway. In any case, every patient will need an individualised care plan. In these, although the degree of frailty is likely to be informative, it cannot be expected to be definitive. Even if care planning is approached in consideration of the degree of frailty, one solution will not fit every patient.
Work on frailty cannot occur in isolation. It must fit with a health care system’s strategic plan. Such plans typically recognise the need to deliver a high-quality and sustainable system. In this context, it is not difficult to cite addressing the complex challenge of frailty as a central means of meeting such an objective. Very commonly too, health care systems espouse the need to strengthen and support a high-performing workforce. Helping them understand frailty and incorporate it into care planning means supplying them with the tools that they need, which for an ageing population will include frailty assessment.
How best to improve care for people living with frailty (all at once, or incrementally) will vary by setting. Everywhere, finding an optimal means of ‘geriatricising’ routine care must be considered and evaluated. Even so, a critical variable will be cultural: how prepared is a system or institution to grapple with the concept of frailty? For example, UK proposals to focus on delivery of Comprehensive Geriatric Assessment within 72 hours of presenting in urgent care settings26 or on hospital-wide geriatric assessment27 do not seem as fantastical there as they would in any North American jurisdiction. Even in North America, system-wide changes delivered through locally contextualised interventions can be effective.28 As reforming care for people living with frailty contains an at least implicit critique of how care is provided now, acceptance is made easier by usable tools that are available on a cost-effective, real-time basis, and are easily communicated. The data arising from them must seamlessly link across elements of health care (public health, primary care, various types of community, prehospital, hospital and long-term care) with the clear aim of improving outcomes.
System change requires extensive discussion and consultation, balanced against the need to get started. If particular groups seem to have made some headway, they often can provide a focus for getting start. That is easiest for teams that might welcome evaluation with a view to more widespread adoption of the techniques which they have found to work in their community of practice. Even so, how to scale will be a function of ease of use, ability to reliably identify people living with frailty, and uptake. Commonly such an orientation – to build on local successes - favours an incremental approach. It also helps to de-risk decision-making, reducing the reluctance to change too much too soon, while reinforcing the knowledge that not changing at all is no longer an option.
Interventions are needed across health care settings. Both comprehensive29 and more local responses (such as the mobilisation initiatives being carried out across Ontario28) can be adopted. Proof of concept consists first in showing that an intervention can work, and then understanding both conditions that lead to success, and conditions in which both system and patient goals are not met. Controlled trials have some role in this, but their ability to exclude the very patients who need to be studied, and the infeasibility arising from time taken to devise protocols, get them funded and have them pass ethical review militate against an exclusive reliance upon them. Into this turbulent surf, Quality Improvement initiatives built on Plan-Do-Study-Act cycles have waded. Their advantages are many, but that does not mean they are without problems; here again, system and institutional cultures will be crucial to getting the best use from such efforts.30
As healthcare practitioners will know, change is difficult. They will also know that populations are ageing, and that what we have done for so long works less well now. A focus on frailty offers a comprehensible way to understand how this has come about, and how we can respond.
Giants are large and powerful. If they are to be confronted, they must be taken seriously. For this, recognition is an essential first step."
- Kenneth Rockwood (2016)