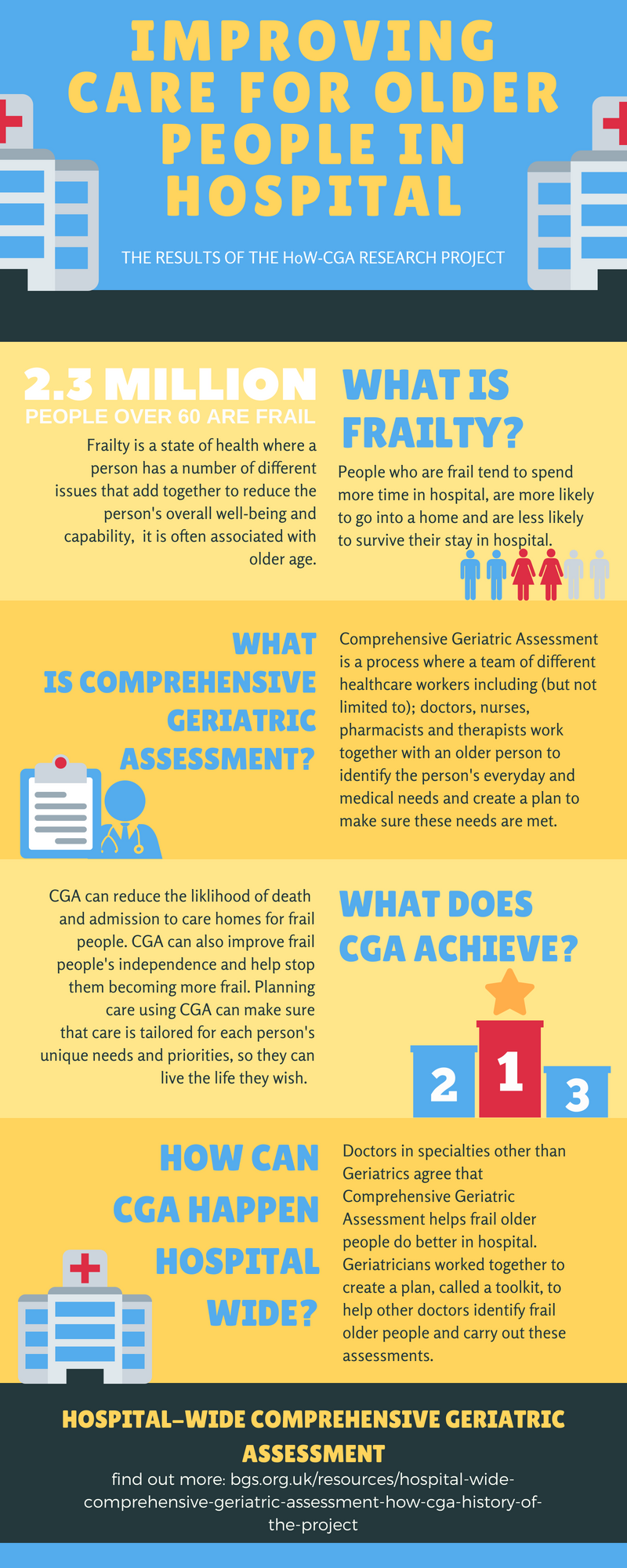
What is Frailty and why is it important?
Frailty is a state of health where a person has a number of different issues that add together to reduce the person’s overall well-being and capability and, is mostly associated with older age. People who are frail tend to spend more time in hospital, are less likely to return to their own home, are more likely to need care support if they do go home and are also less likely to survive their stay in hospital.
What is Comprehensive Geriatric Assessment?
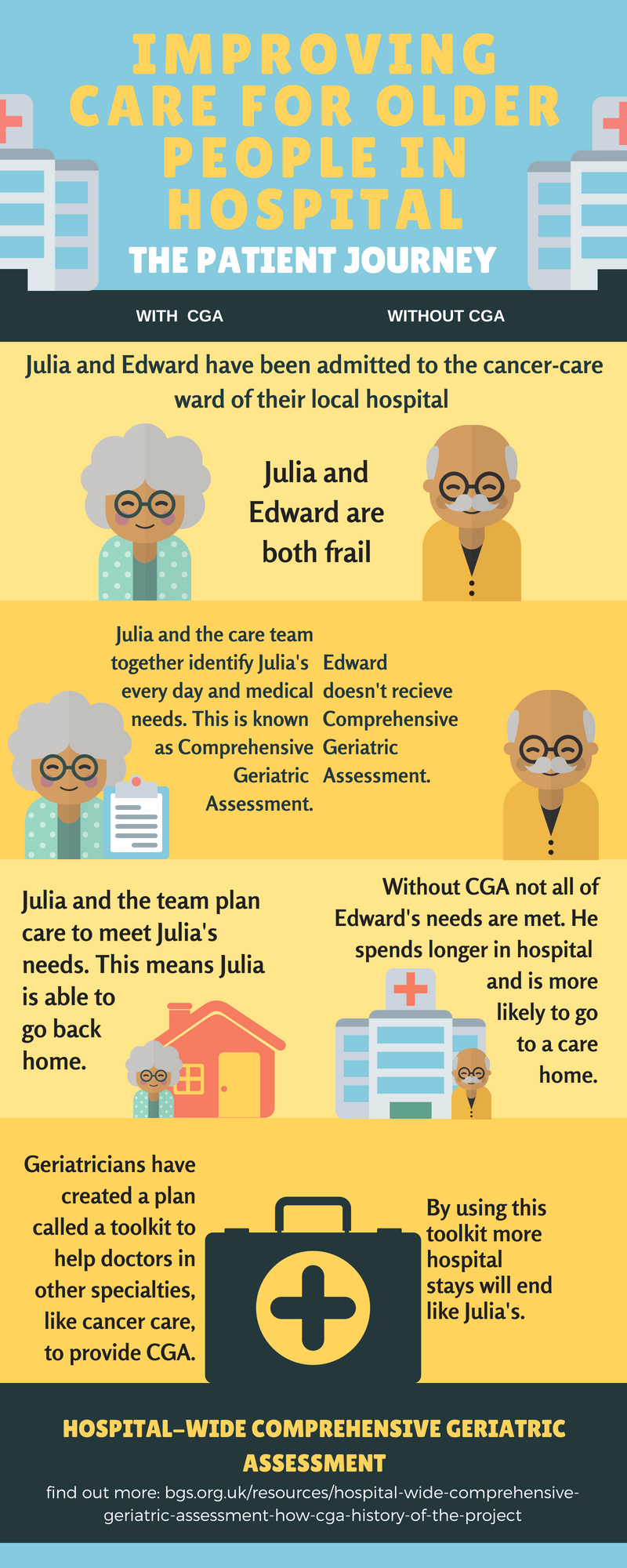
Research has shown that identifying people who are frail in hospital allows each frail person’s individual needs to be identified and then steps can be made by care teams to meet those needs. To do this a frail person can undergo Comprehensive Geriatric Assessment (CGA). CGA assess many aspects of a person’s health and wellbeing. Some examples of the many things assessed by CGA are a person’s risk of having a fall, extra help or care they might need at home and how able they are to do the everyday things that are important to them (e.g. cooking and washing). Currently, CGA is usually carried out by teams who specialise in the care of older people. The researchers in the HoW-CGA project proposed that teams in other specialties across a hospital would be able to carry out CGA for frail people in their care and that this would help improve the care a frail person received and help meet the person’s needs.
What are the aims of the HoW-CGA project?
The HoW-CGA project had four main aims:
Aim 1
The first aim of the project was to define what CGA is. To do this the team conducted a literature review, a research technique that involves reading research that already exists in databases, to find out how other researchers define CGA. The most common definition of CGA the team found was: “a multidimensional, multidisciplinary process which identifies medical, social and functional needs, and the development of an integrated/coordinated care plan to meet those needs.”
This essentially means that CGA is a process that is made up of lots of different elements and involves lots of different members of hospital staff (such as doctors, nurses and therapists). CGA identifies a person’s medical needs, as well as needs they may have outside of hospital such as accommodation or care they might need at home and, needs they may have in going about their day to day life such as walking aids or special adaptations to their homes. CGA enables members of staff to create a clear plan for how to meet these needs and how everyone can work together to make sure the plan is carried out.
Aim 2
The second aim of HoW-CGA was to find out where CGA already takes place, how it is done, what the outcomes of CGA are and how much it costs. To find out this information the researchers created a large survey which was sent out to hospitals around the country. 58 hospitals answered questions in the survey such as ‘Does the hospital assess frail patients?’ and ‘Does the hospital always assess frail people in the same way?’ From the responses the team discovered that hospitals were often good at finding out about frail people’s memory and brain function, how able people were when walking and if they were likely to fall, people’s medicines, and whether people had any problems with bladder and bowel control (continence). The survey showed that hospitals could improve in finding out about and treating people’s mood and making sure they didn’t lose their continence.
The research also looked at how much it would cost to carry out CGA. The research team did this by working with experts to calculate costs of different scenarios for different types of patients. They found out that performing CGA would cost the hospital between £90 and £172 more per person. The overall cost of a frail person being in hospital is about £2000-£3000 so this was only about a 5% rise in cost. The aim of CGA is to make sure that a person’s needs are met and so make them less likely to need to go back to hospital in the future which should ultimately save more money in the long run.
Aim 3
The third aim of the project was to find out what types of people usually undergo CGA and which of these people benefit from them. To do this the team analysed a large amount of data from existing research. They found out that 3/4s of people over the age of 75 visited hospital at least once which rose to nearly 100% of people over four years. They found that frail older people were more likely to have lots of needs that could be identified by a CGA and then met by the team caring for them.
Aim 4
The fourth and final aim of the project was to create a ‘toolkit’ or ‘instruction manual’ that would enable non-geriatric teams to conduct CGA for a person they think might be frail and who they feel would benefit from a care plan like the ones outlined above. The researchers used interviews and observations to find out what support staff needed in performing CGA for someone.
From all of their research the team created a plan known as a ‘toolkit’ to support staff when carrying out CGA and tested it out in three hospitals. The hospital teams who tested out the toolkit all thought that CGA would be very beneficial to many people in their care. The teams did find that sometimes CGA was not their first priority when caring for people (i.e. they found they were too busy) and they sometimes needed support from geriatricians in their hospital when carrying out CGA. It is hoped that over time and by using the toolkits, staff will get better at CGA for people and they will become part of teams’ normal routine when caring for frail patients.
Overall, the majority of older people attend hospital at some point in their life and the more frail a person is the more likely they are to be admitted to hospital. These are the people that the HoW-CGA project found would benefit from CGA. The toolkit will help care teams ensure more people receive CGA which will hopefully improve those people’s care. As time goes on the researchers can follow up the progress of the teams using the toolkits and find out how they have benefitted frail people in hospital.